Since 1936 TMJ has been primarily treated by dentists, however today, we know TMJ to be a complex condition with many biological systems (circulatory, digestive, endocrine, exocrine, immune, muscular, nervous, reproductive, respiratory, and skeletal) playing a role, indicating the need to bring the medical and other allied health professionals in research and patient care.
There are no formally developed standards of care for TMJ in clinical dentistry or medicine. Although a variety of health care providers advertise themselves as “TMJ specialists,” most of the more than 50 different treatments available today are not based on scientific evidence of safety and efficacy. These doctors practice according to one of many different schools of thought on how to best treat TMJ.
Jump to a Section Below
Seeking TMJ Care
If your TMJ problem gets worse with time, you should seek professional advice. Proceed cautiously, and get several independent opinions before beginning any suggested irreversible treatment.
It’s important to first rule out other conditions that may mimic TMJ symptoms by consulting your medical doctor. For example facial pain can be a symptom or a result of conditions, such as:
- sinus or ear infections
- decayed or abscessed teeth
- various types of headache
- facial neuralgia (nerve-related facial pain)
- tumors
- oral and jaw bone cancers
- connective tissue disorders such as Ehlers Danlos Syndrome and Scleroderma
- Eagles syndrome
- Dystonia
- Lyme Disease
The National Institutes of Health (NIH) advises patients to look for a health care provider who understands musculoskeletal disorders (affecting muscle, bone and joints) and who is trained in treating pain conditions. Pain clinics in hospitals and universities are often a good source of advice, particularly when pain becomes chronic and interferes with daily life.
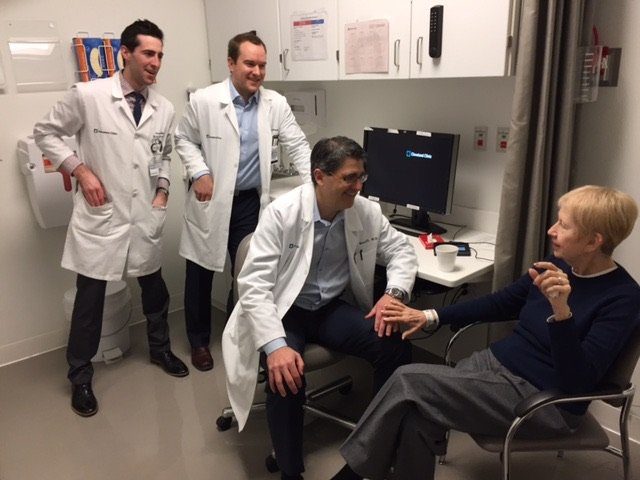
Complex cases, often marked by chronic and severe pain, jaw dysfunction, comorbid conditions, and diminished quality of life, will likely require a team of doctors from fields such as neurology, rheumatology, pain management, and other specialties for diagnosis and treatment.
Be Informed
First and foremost, educate yourself. Informed patients are better able to talk with health care providers, ask informed questions, and make knowledgeable decisions. When going to the doctor, it is in the best interest of every patient to always be accompanied by a person whom you trust and who will act as your advocate. We recommend taking notes during your appointments.
Here are some questions you should ask before consenting to treatment.
- What is the purpose of the treatment, and why is it necessary in my case?
- Is the treatment reversible, or is it irreversible?
- What other treatments are available?
- Will this treatment improve my condition?
- What side effects or complications may occur and how will they be addressed?
- What are the advantages of the proposed treatments rather than other forms of therapy with respect to benefits and risks?
- How many follow-up treatments or visits will be necessary?
- How much will the treatment cost?
- Will insurance cover the treatment costs?
- Is there a payment contract I must sign? (If so, ask to take the form home to review.)
- Is there a consent form I must sign for treatment? (If so, ask to take the form home to review.)
- Has the treatment been studied in clinical trials* for safety and effectiveness?
- Is this treatment part of a clinical trial*? If so, what are my obligations and the conditions involved in participating in this trial?
Clinical Trials
If you are offered a clinical trial*, feel free to ask any questions or bring up any issues concerning the trial at any time. The following suggestions may give you some ideas as you think about your own questions.
The Study
- What is the purpose of the study?
- Why do researchers think the approach may be effective?
- Who will fund the study?
- Who has reviewed and approved the study?
- How are study results and safety of participants being checked?
- How long will the study last?
- What will my responsibilities be if I participate?
Possible Risks and Benefits
- What are my possible short-term benefits?
- What are my possible long-term benefits?
- What are my short-term risks, such as side effects?
- What are my possible long-term risks?
- What other options do people with my disease have?
- How do the possible risks and benefits of this trial compare with those options?
Participation and Care
- What kinds of therapies, procedures, and/or tests will I have during the trial?
- Will they hurt, and if so, for how long?
- How do the tests in the study compare with those I would have outside of the trial?
- Will I be able to take my regular medications while participating in the clinical trial?
- Where will I have my medical care?
- Who will be in charge of my care?
Personal Issues
- How could being in this study affect my daily life?
- Can I talk to other people in the study?
Cost Issues
- Will I have to pay for any part of the trial, such as tests or the study drug?
- If so, what will the charges likely be?
- What is my health insurance likely to cover?
- Who can help answer any questions from my insurance company or health plan?
- Will there be any travel or child care costs that I need to consider while I am in the trial?
Tips for Asking Your Doctor About Trials
- Consider taking a family member or friend along for support and for help in asking questions or recording answers.
- Plan ahead what to ask, but don’t hesitate to ask any new questions you think of while you’re there.
- Write down your questions in advance to make sure you remember to ask them all.
- Write down the answers, so that you can review them whenever you want.
- Ask about bringing a tape recorder to record what’s said (even if you write down answers).
Tips for Talking to Your Doctor
Your health care provider should answer these questions in words you can understand. If you don’t understand any part of the discussion with your health care professional, it is important to ask that it be explained again. If your provider will not or cannot answer these questions, find one who will. You must be your own health care advocate:
- Speak honestly and openly.
- Be clear and specific about your TMJ issues.
- Discuss any or all pain you are experiencing.
- Ask questions if you don’t understand.
- Ask about all treatment options.
- Ask your doctor to explain any treatments.
- You can say no to any test, treatment or request.
- Your health care professional’s job is to help you. Keep in mind that your doctor working for you. Make sure the visit focuses on you and your needs.
- Make your own choices about what steps to take.
- Get other opinions before making decisions.
- Be confident. If you feel uncomfortable with your doctor, change health care professionals.
- If fees seem excessive, you can ask about them and compare with other providers.
- If you think it will be a difficult discussion, ask someone you trust to accompany you to the office visit. This person can take notes, ask questions, make sure you have addressed all the points you wanted to make (sometimes during stressful office visits important things fall through the cracks). Even for routine visits it is always beneficial to have a second set of ears in the room.
Throughout Your Treatment
- Some people find it helpful to keep a diary of pain and other symptoms. A diary can help when you talk to your doctor.
- Keep a record of you symptoms, when you experience them, what may trigger them.
- Pay attention to what makes you feel better or worse.
- Keep a record of what times of day you feel worse.
- If you have X-rays, MRIs or other test results, bring them with you to your appointments if possible. Your medical and dental records belong to you, and you can ask for copies of these records.
- If medication is prescribed, be sure to ask about its side effects.
