Orofacial Pain: Prospective Evaluation and Risk Assessment (OPPERA)
Table of Contents
Study Findings
This revolutionary, first-of-its-kind, multi-site study – funded by the National Institute of Dental and Craniofacial Research and directed by late William Maixner, PhD, DDS, the Director of Center for Translational Pain Medicine at Duke University – is the first and only prospective, longitudinal study of temporomandibular disorders (TMD) to date to enroll and monitor over 4,000 men and women over a 5-year period. It identified risk factors, signs, symptoms, genetic factors and environmental events that contribute to the development and chronicity of painful TMJ disorders. (see Figure 1) OPPERA also aimed to understand the factors that predict the transition from the acute to chronic TMJ disorders, as well as the development of chronic overlapping pain conditions, including headache, low back pain, irritable bowel syndrome and widespread body pain.
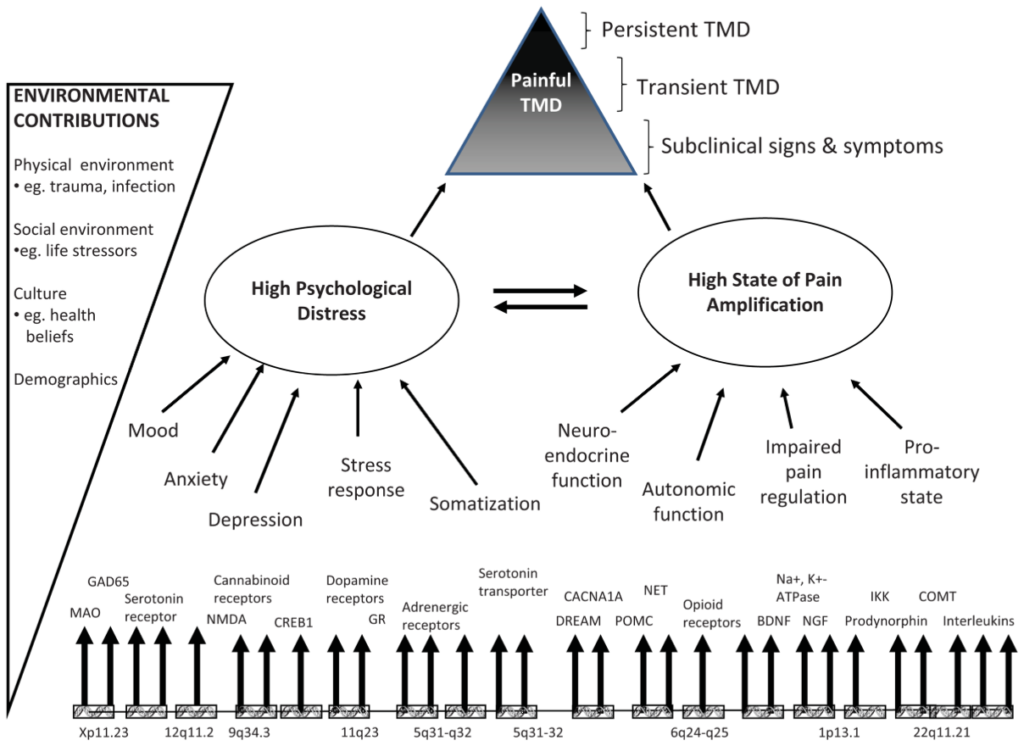
Figure 1. This model displays two principal intermediate phenotypes (psychological distress and pain amplification) that contribute to onset and persistence of TMD. Each intermediate phenotype represents a constellation of more specific risk factors, all of which are subject to genetic regulation. Interactions between intermediate phenotypes take place in the presence of environmental contributions that further contribute to onset and persistence of painful TMD. Time is not shown in the model, because its effects occur implicitly on a third dimension that is not readily shown in the diagram.
Since OPPERA’s first publication in 2011, over 30 papers summarizing the study’s expansive findings collectively demonstrate that TMJ is a complex condition with a biopsychosocial model of illness, and that it is no longer appropriate to regard TMJ disorders as a localized jaw/dental condition.
OPPERA’s initial major findings include:
- TMD is a prevalent condition – 4% of the OPPERA study population developed TMD on an annual basis
- TMD prevalence was highest in those aged 35-44 years (~7%) and the least in those 18-24 years (~3%)
- Women were 4 times more likely than men to develop TMD
- TMD was more prevalent in non-Hispanic whites, compared to African Americans and Hispanics
- People who developed TMJ disorders (or had chronic TMJ) were more likely to have the following signs and symptoms:
- Diminished ability to chew, reduced mouth opening and reduced jaw function
- Increased sensitivity in the cranial (or skull) muscles
- Increased number and severity of “somatic symptoms” (e.g., stomach/bowel problems, headaches, chest pain, shortness of breath, dizziness, feeling tired or having low energy, trouble sleeping) – which may indicate that people with TMJ disorders have a dysfunction in how their bodies regulate sensory function
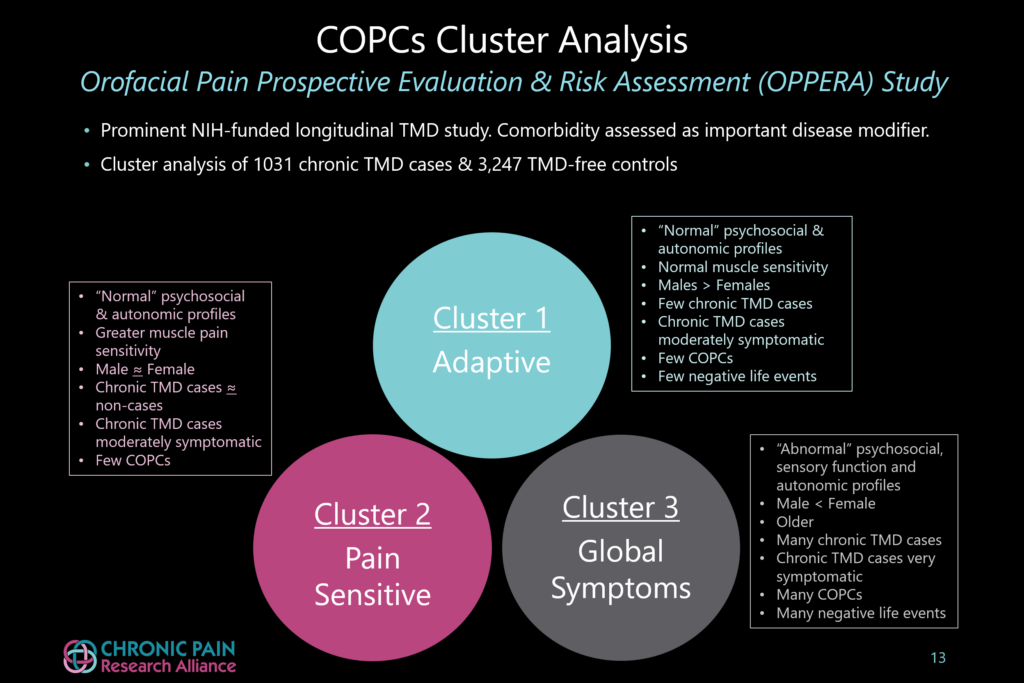
- TMJ is not just one condition, but a mix of conditions. (see Figure 2) OPPERA identified at least 3 distinct groups that vary in symptom severity and number of chronic overlapping pain conditions (COPCs):
- Group 1 (“Adaptive”): Patients in this group report less severe pain, very little psychological distress and have the least muscle pain sensitivity. Pain is localized to the temporomandibular joint and surrounding muscles with very few COPCs. More men than women fall into this group.
- Group 2 (“Pain Sensitive”): People in this group show the greatest sensitivity to muscle pain, have slightly greater psychological stress and more COPCs, compared to Group 1. This group contains slightly more women than men.
- Group 3 (“Global Symptoms”): TMJ patients in this group have the most severe pain and dysfunction. They have more tender muscle sites and many more COPCs, as well as experience the greatest psychological distress. This group is also less able to control cardiovascular function compared to the other two groups. People in this group experience a greater history of jaw injury and traumatic life events. A higher percentage of patients have a history of smoking. Many more women than men fall into this group.
7. OPPERA also identified several environmental and life events that are associated with the risk of developing TMJ disorders and chronicity. They include a history of jaw injury, lifetime history of smoking, contraceptive use and traumatic life events.
8. Findings from OPPERA’s ongoing genetic and genomic studies have identified several disrupted biological pathways related to pain processing, inflammation, immune function and psychological function, demonstrating that TMJ disorders should be considered a multi-system illness rather than an isolated jaw/dental condition. Many of these dysfunctional pathways are targets of intense investigation and researchers are already identifying medications that may prove useful in treating different groups of TMJ patients (with and without COPCs). Many of the medications under investigation influence serotonin, stress hormones (such as epinephrine) and immune function. Several drug targets have been identified and new pharmacological and non-pharmacological therapies for TMJ disorders and related conditions are on the horizon.
